Prehabilitation has been shown to reduce the recovery time period and complications after surgery. The general conditioning that can be incorporated into a Prehab program can offset some of the detrimental side effects of these procedures the patient is better prepared and can handle it.
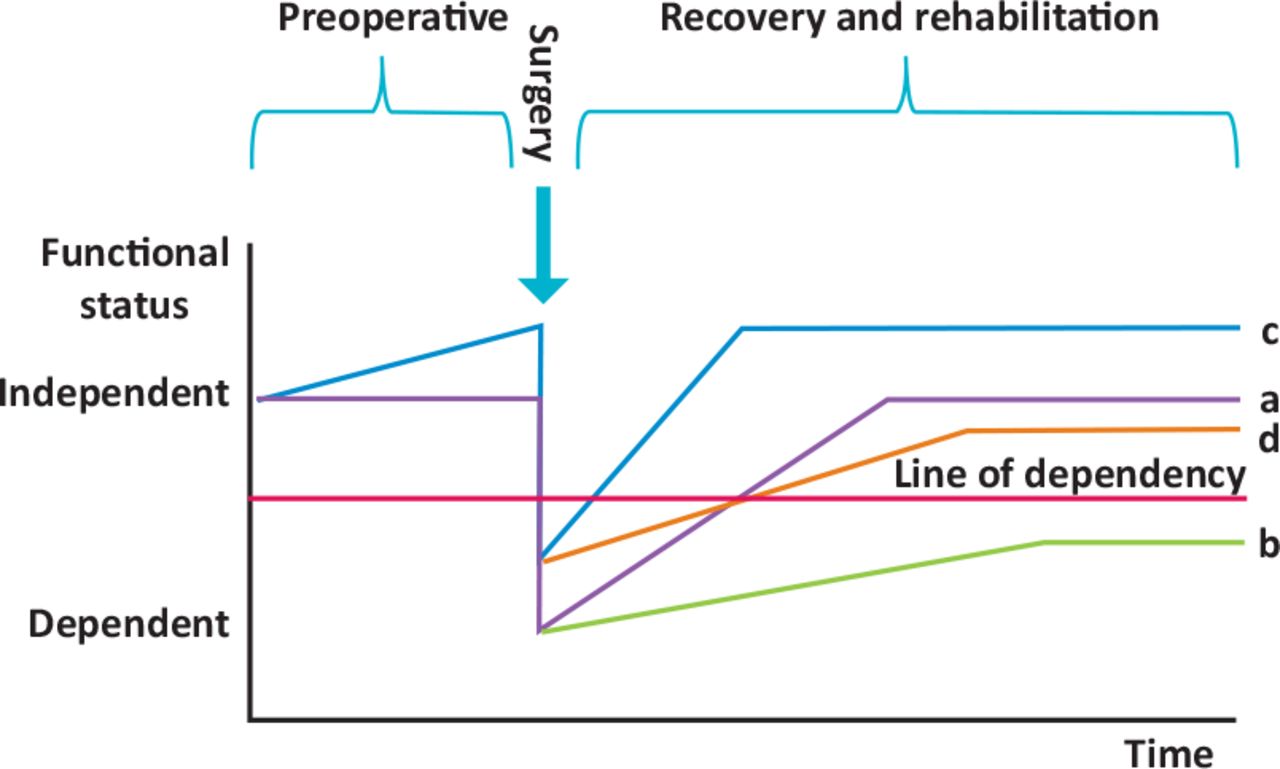
- Prehabilitation programs are designed to enhance the fitness and functional level of the patient prior to undergoing their procedure.
- Prehab programs have been successful at reducing the post-operative time period.
- Patients have reported less anxiety towards their medical procedure when they have participated in a Prehab program.
- Prehab programs have been shown to be successful when they consisted of a minimal 30 minute bout of specific exercises.
- Seek the advice and treatment from a Physical Therapist for a sound Prehabilitation program .
Implementing Prehab
Prehab and Lifestyle Medicine
• Pillars of lifestyle medicine
– Quality of life
– Disease prevention
– Baseline testing
– Prescriptive exercise
– Saving overall health care dollars
• Formal prehabilitation is a perfect way to begin this engagement of opportunity
Prehab to Different Parties
• Prehab to the patient: this is when a “possible” event becomes a planned event and they begin the work to prepare physiologically with activity, nutrition, sleep habits
• To the rehab provider: we are initiating our care earlier and getting to establish a true baseline functional status as well as optimize both the patient and ourselves for the post-event (surgery, chemotherapy) course of treatment
To the surgical/medical team: prehab is an opportunity for them to work with a patient who is calmer, more physically ready, and therefore decrease complication/readmission rates
• To the healthcare system/hospital: this is a silver spoon to avoid re-admits
– In 2016, the Mary-Washington Regional Cancer Center won the ACCC Innovator Award for a pilot of just six patients completing lung cancer prehab: largely due to the demonstrated decrease in length of stay post surgically
– Decreasing burden on the system as a whole with prehab
Assessments Specific to the Patient Impairment
Potential items to include/consider
– Balance
– Cardiorespiratory fitness
– Sensation
– Functional mobility
– Edema/lymphedema
– Memory/acuity
– Pain
– Fatigue level
– Strength
– Joint assessment
– Sexual function if indicated
– Health related quality of life
Prehab Outcomes
• Small case reports and cohorts report improvement in
– Walking ability and distance
– Stamina and decreased fatigue
– Surgical complications
– Hospital length of stay: small “N”
• Generally, prehabilitation programs are diverse in their application of intervention as well as duration, frequency, and intensity of oversight which is a
challenge when engaging a healthcare system
Outcomes: What Can Be Achieved?
• RCT volume is low but first publication in 144 high-risk patients 1
• Randomized to control (education) or prehabilitation for four to six weeks, multi modal
– General exercise
– Supervised Specific moderate intensity exercise
– Motivational interviewing
• Benefit was shown to enhance post operative outcomes of aerobic capacity, and decreased acute complications by 51%
• Individualized care maximized impact
Clear Expectations
• Set clear expectations with the medical team and the patient based on your available time for prehab
• Most prehab programs are demonstrating success between eight to ten visits for ambulation ability and decreased time to return to baseline function
• What we can’t say with certainty is
– Whether or not any preoperative increase in function with offset the postoperative morbidities and from sequential therapies
Summary
• Prehab is one of the first, non-reactionary opportunities to engage in lifestyle medicine
• Physical therapists possess a unique set of skills, and time, to engage patients in their overall health
• Prehab is medical care offering individualized and prescriptive interventions
• A variety of patient populations can benefit from prehab including surgical cases, chronic illness preparing for intervention, and high risk populations
• Connect and negotiate with community resources, making wellness mutually beneficial to all parties
SOURCE: Medbridge
Ace Physical Therapy and Sports Med Institute
Additional Facts:
Knee Score was significantly different between the two observed groups postoperatively, 3 months postoperatively and 6 months postoperatively, while the Function Score was not significantly different in that period. Prehabilitation program provides better preoperative KS and FS, and better KS up to 6 months postoperatively.
The hospital length of stay was shorter by one day, with a median (middle value) of six days for participating patients versus seven days for controls, who received no prehabilitation. Program participants were more likely to be discharged from the hospital to home: 65.6 percent versus 57 percent of controls. Medicare paid nearly $3,200 less in total payments for both hospital and posthospital care (what Medicare calls an “episode of care”) for patients who underwent prehabilitation than for controls: $31,641 versus $34,837. Insurance payments were especially lower among patients for posthospital care, including skilled nursing facility ($941 versus $1,566 for controls) and home health care ($829 versus $960 for controls).
SOURCES:
- Jahic D, Omerovic D, Tanovic AT, Dzankovic F, Campara MT. The Effect of Prehabilitation on Postoperative Outcome in Patients Following Primary Total Knee Arthroplasty. Med Arch. 2018;72(6):439–443. doi:10.5455/medarh.2018.72.439-443
- James Durrand, , A Statewide Prehabilitation Program and Episode Payments in Medicare Beneficiaries, Journal of the American College of Surgeons. DOI: https://doi.org/10.1016/j.jamcollsurg.2019.10.014.
